轻微肺部感染患者使用抗生素治疗无效
阿莫西林是常用的抗生素,常用来治疗轻微肺部感染。最新研究发现,抗生素对轻微肺部感染的持续咳嗽患者治疗无效,即使是在老年患者。本研究发表在12月19日在线出版的《柳叶刀传染疾病》。
这是迄今抗生素治疗下呼吸道感染最大的以安慰剂对照的的随机临床试验。来自欧洲12个国家2000余例急性下呼吸道感染患者(持续咳嗽≤28天)参与了此项研究。研究随机分为两组,一组接受抗生素治疗(N=1038),另一组接受安慰剂治疗(N=1023),安慰剂组使用糖片的惰性治疗形式,一天三次,一个疗程服用七天。
抗生素肺部感染
研究发现两组患者在疾病严重程度和持续时间上几乎没有差异,即使在老年患者(年龄在60岁或60岁以上的患者)也是如此。领导该研究的英国南安普敦大学PaulLittle教授说:“与不服药患者相比,服用阿莫西林的患者并不会更快地恢复或减轻症状。事实上,对疑似未患肺炎的患者使用抗生素阿莫西林治疗呼吸道感染,非但不利反而有害。按照初级处方(大多是基层医生开出),过量使用抗生素,尤其当它们无效时,会导致出现耐药性且有副作用,如腹泻、皮疹和呕吐。我们的研究结果表明,患者自己就会恢复好。但抗生素对少数患者会有效,问题是如何找出受益于抗生素的人,这仍具挑战性。”
欧洲疾病预防与控制中心(ECDC)最近发表声明称,抗生素耐药性仍然是全世界公共健康的一个主要威胁,很大程度上是由于滥用抗生素。肺部感染,也称下呼吸道感染,是发达国家基层医疗单位最常见的急性疾病。对下呼吸道感染患者是否应该用抗生素治疗现在仍然存在争议,尤其是在年长患者,因为大多数下呼吸道感染主要是病毒感染所致。但专家警告称,若怀疑是肺炎,出于严重性考虑,仍应使用抗生素。
在一篇评论中,来自瑞士巴塞尔大学的菲利普教授指出:“Little和他的同事们提供了令人信服的数据,应该鼓励基层医疗单位的医生,在低风险疑似未患肺炎的患者中避免使用抗生素治疗。然而这种一刀切的方式能否能得到进一步改善呢?或许检测细菌感染的特殊血液标志物,以识别那些少数能受益于抗生素的人是一种更优方法,既能避免副作用,又能防止出现抗生素耐药。”
皇家学院全科医生迈克尔.摩尔博士,也是这项研究的合著作者,他也表示:“重要的是全科医生们清楚地知道,他们应不应该给病人开抗生素,从而减少社区细菌性耐药的发生。
Amoxicillin for acute lower-respiratory-tract infection in primary care when pneumonia is not suspected: a 12-country, randomised, placebo-controlled trial
Background
Lower-respiratory-tract infection is one of the most common acute illnesses managed in primary care. Few placebo-controlled studies of antibiotics have been done, and overall effectiveness (particularly in subgroups such as older people) is debated. We aimed to compare the benefits and harms of amoxicillin for acute lower-respiratory-tract infection with those of placebo both overall and in patients aged 60 years or older.
Methods
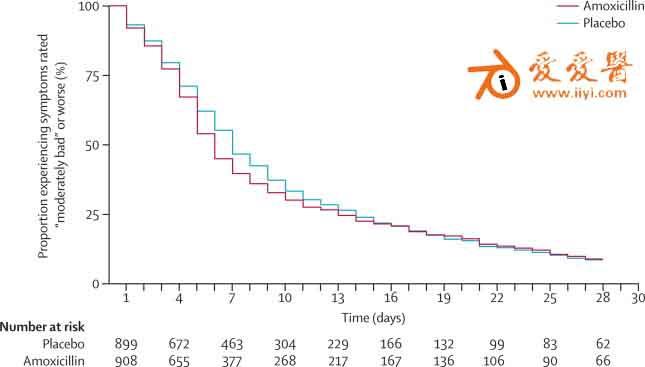
Patients older than 18 years with acute lower-respiratory-tract infections (cough of ≤28 days' duration) in whom pneumonia was not suspected were randomly assigned (1:1) to either amoxicillin (1 g three times daily for 7 days) or placebo by computer-generated random numbers. Our primary outcome was duration of symptoms rated “moderately bad” or worse. Secondary outcomes were symptom severity in days 2–4 and new or worsening symptoms. Investigators and patients were masked to treatment allocation. This trial is registered with EudraCT (2007-001586-15), UKCRN Portfolio (ID 4175), ISRCTN (52261229), and FWO (G.0274.08N).
Findings
1038 patients were assigned to the amoxicillin group and 1023 to the placebo group. Neither duration of symptoms rated “moderately bad” or worse (hazard ratio 1·06, 95% CI 0·96–1·18; p=0·229) nor mean symptom severity (1·69 with placebo vs 1·62 with amoxicillin; difference ??0·07 [95% CI ??0·15 to 0·007]; p=0·074) differed significantly between groups. New or worsening symptoms were significantly less common in the amoxicillin group than in the placebo group (162 [15·9%] of 1021 patients vs 194 [19·3%] of 1006; p=0·043; number needed to treat 30). Cases of nausea, rash, or diarrhoea were significantly more common in the amoxicillin group than in the placebo group (number needed to harm 21, 95% CI 11–174; p=0·025), and one case of anaphylaxis was noted with amoxicillin. Two patients in the placebo group and one in the amoxicillin group needed to be admitted to hospital; no study-related deaths were noted. We noted no evidence of selective benefit in patients aged 60 years or older (n=595).
Interpretation
When pneumonia is not suspected clinically, amoxicillin provides little benefit for acute lower-respiratory-tract infection in primary care both overall and in patients aged 60 years or more, and causes slight harms.







